‘I could have an $80,000-a-year career, but this is more important’
BRISTOL – Lynn and John Patton sit in their living room, cradling the box that contains the ashes of their son, Matthew, who was an Army sergeant.
Matthew died by suicide on May 13, 2013, three years after he had deployed to Afghanistan. He was a troubled man when he returned, the Pattons told Ocean State Stories.
“He just wasn’t himself,” said Lynn. “Before, he was always laughing and doing all these stunts and goofing around on people but he wasn’t doing any of that. He was very quiet. He was having nightmares.”

On leave from his base at Fort Hood Texas, Matthew was visiting an Army friend in North Carolina when he took his life with a gun. The friend did not witness it. Matthew was 23.
Although Matthew had experienced mental health challenges when he was a child, the shock to the Pattons and their three other children was profound.
“Mother’s Day was the last time I talked to him,” said Lynn a registered nurse.
“We all talked to him,” recalled John, an engineer.
“I knew something was wrong,” Lynn said, “but he would not tell me what.”
When the family learned of Matthew’s passing, “my brain health suffered with depression and anxiety and PTSD,” Lynn said. John suffered, too.
Matthew’s body was flown to Rhode Island T.F. Green International Airport, where the Pattons met his flag-draped coffin. His funeral service was held on May 25, 2013, at the George C. Lima Funeral Home in Bristol, where Matthew had attended Mt. Hope High School, graduating in 2008, two months before he enlisted in the Army.

As time passed and their own mental health improved, the Pattons came to believe that grief from their son’s death could be channeled into an effort to help other active-duty military members and veterans – and so they founded the Matthew Patton Foundation, an educational and advocacy organization aimed at enhancing mental health and preventing suicide.
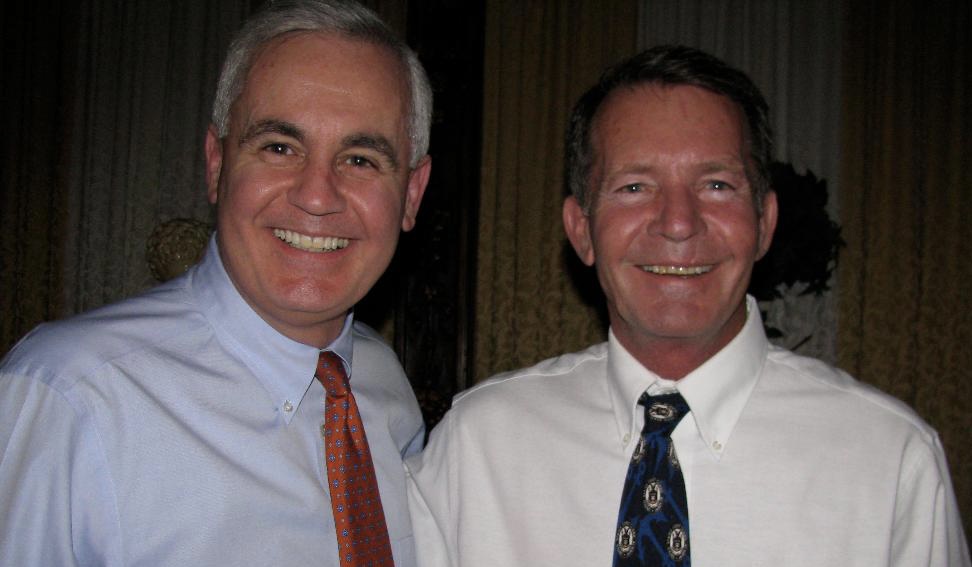
The Pattons say the foundation, whose board of directors and advisory board includes Army, Navy and Marine veterans, has succeeded.
“I could have an $80,000-a-year career, but this is more important,” Lynn said. “I make no money saving lives but I’m a millionaire every life I save.”
With Veterans Day approaching, Larry Connell, director of the VA Providence Medical Center, invited Ocean State Stories to visit the center’s Mental Health Center, Building 39 on the center’s sprawling campus on Chalkstone Avenue, to learn about the VA Healthcare System’s local and national initiatives aimed at preventing veteran suicide.
That effort, Connell said, is “the whole VA’s number-one clinical priority.”
A native Rhode Islander and University of Rhode Island graduate, Connell joined the Army in 1985 and became a highly decorated medical service officer and medical evacuation helicopter pilot. He retired from the service as a colonel in 2015, after duty that included participation in Operation Desert Storm, the 1991 campaign that freed Kuwait from Iraqi occupation.

“I’ve seen some pretty nasty things in combat,” Connell said. It gave him a keen appreciation for issues facing many veterans.
Connell cites the latest statistics compiled by the U.S. Department of Veterans Affairs’ Office of Mental Health and Suicide Prevention and published in its 2021 annual report that show an average of 17 veterans dying every day by suicide. Another three active-duty service members die daily that way, according to Connell. Many but not all have seen combat.
“Of those 17 veterans that die every day, more than half of them have not either enrolled or been to the VA in the previous year for care,” Connell said. “So if we could somehow get our arms around those veterans and bring them back in to get them the help they need we really we could bend that needle down,” making further progress.
The “somehow” is actually a national initiative designed “to end Veteran suicide through implementing a public health approach that combines both community-based and clinically based strategies across prevention, intervention, and postvention areas of focus,” according to the VA’s 2021 annual Veteran Suicide Prevention Report.
In Rhode Island, as elsewhere, key features of the initiative include:
● Consultation, evaluation, individual and family therapy, psychiatric services, medicine, treatment for addictive disorders, including at residential rehabilitation programs. Inpatient and outpatient services are available, along with telehealth appointments. LEARN MORE.
● Services for veterans who are homeless at risk of becoming so. Services include immediate food and shelter, transitional and permanent housing, life skills development, job training and education, and “support with justice system navigation and community re-entry from jail.” LEARN MORE.
● A range of services to support family members or other who are caring for a veteran. LEARN MORE.
● “Improve lethal means safety,” as stated in the 2022 Prevention report. According to that report, 71% of veteran suicides in 2020 were by firearms (with suffocation accounting for 14.9% and poisoning 8.4%)
Recognizing that a veteran in a suicidal crisis needs immediate attention, the Department of Veterans Affairs in January implemented the so-called COMPACT Act (for Comprehensive Prevention, Access to Care and Treatment Act), which lets veterans go to any VA or non-VA healthcare for no-cost emergency care, “including inpatient or crisis residential care for up to 30 days and outpatient care for up to 90 days,” the department said in announcing COMPACT.
“Veterans do not need to be enrolled in the VA system to use this benefit,” the VA stated in a Jan. 13 press release. “This expansion of care will help prevent veteran suicide by guaranteeing no cost, world-class care to veterans in times of crisis. It will also increase access to acute suicide care for up to 9 million veterans who are not currently enrolled in VA.”
Said Connell: “Let’s say you live down in Westerly. It’s a good hour drive up here to get to the emergency room if you’re a veteran in crisis. While we would love to have them come here for their care, we understand that that may not be convenient, certainly not at one o’clock in the morning.” Westerly Hospital, however, would be minutes away.
“Or say you’re down in Newport and it’s two o’clock in the morning,” Connell continued. “Do I want to drive up to Providence? No, of course not. So I would go to the Newport Hospital emergency room.”
Any Rhode Island hospital with emergency services can be used under COMPACT – and also hospitals in southeastern Massachusetts and Cape Cod, which fall under Providence VA jurisdiction.
Determining who is at risk of suicide is “a very complex issue,” according to Connell. “Some veterans will commit suicide that may not have had any indications, and other veterans that you think would commit suicide don’t.”
Still, experience has demonstrated that veterans with financial issues, marital and relationship difficulties, and combat memories fit the profile of high-risk.
“Veterans of combat certainly have even more complex issues because they’ve seen some pretty horrible things down range,” the director said. “Their buddy may have died and they feel guilty: ‘Why did I live and my buddy didn’t?’
“It can be loss of that camaraderie they had with their fellow brothers in arms in combat. That’s a big indicator, we believe, so we’re trying to do a lot of group therapy with veterans — get them in with veterans that have had similar experiences and talk about their experiences and get them back together with like-minded people.”

Asked what someone should do if they suspect a veteran they know is in crisis, Connell said: “The word we’re trying to get out to everybody is ‘don’t wait, reach out. Get that veteran help.’ So if you’re a veteran and I know you are in crisis, I’m your neighbor… You can call the VA, say ‘my buddy is acting real strange. I want to make sure that he gets the help he needs.’
“Our mental health guys will reach out to you: ‘Hey listen, I just want to let you know why don’t you come on in to talk to us. We’ll get you the help you need, make sure you’re enrolled in the Providence VA. Let us get the help you need.’ And that’s the new campaign in the VA: Don’t wait, reach out.”
Although it is too early yet to judge the long-term success of the VA’s suicide prevention programs, preliminary data suggest they are proving effective. According to the department, 6,001 veteran deaths by suicide were recorded in 2001 and they reached 6,796 in 2018, then dropping to 6,146 in 2020, the latest year for which complete statistics are available.
“We’re doing something, right because the numbers are coming down,” Connell said. “They’re not coming down drastically but they are coming down.”

As a child, Matthew Patton “was the happiest kid… very sharing” — and also a daredevil, his mother said.
“For example, our next door neighbor had trees and he cut them off at the top so they didn’t grow and he’d climb up there and sit on top and wave to me and of course, I’d have a heart attack,” Lynn recalled.

But by middle school, Matthew had changed. He began to experience anxiety and depression.
“He had three suicide attempts prior to joining the Army,” Lynn said. Matthew entered into therapy and was placed on medications and his mother left her job as a nurse at Women & Infants Hospital to help care for him. Matthew made it through high school and, along with several of his friends, decided to enlist in the Army. According to the Pattons, his mental health struggles should have disqualified him.
“This aggravates me because his recruiter was a nurse and waved him through,” Lynn said. “The worst thing was Matthew falsified his medical records and did not put any of his history down.” According to Lynn, the Pattons would later learn that while in the Army, Matthew had again attempted suicide. But they were not informed at the time, Lynn said.
Two years after their son died, the Pattons incorporated the Matthew Patton Foundation as a 501(c)(3) non-profit organization. It relies on support from fundraisers and individuals and organizations, which they list on their website. Lynn and John draw no salaries.
The website also chronicles the foundation’s activities, which in the first three years included presentations to 475 soldiers at Matthew’s home base, Fort Hood in Texas; another 60 soldiers during two visits to Fort Bragg, now called Fort Liberty, in North Carolina; and a trip to Hanscom Air Force Base in Massachusetts to discuss suicide prevention with National Guardsmen. As the years have passed, the number of presentations has continued to grow.
So, too, has the foundation’s website. It now includes detailed information about PTSD, depression and anxiety, traumatic brain injury, substance use disorder and suicide, with a “credible resources” page for each that spells out help and treatment options.
The foundation’s annual reports chronicle individual interactions with veterans and soldiers and their families and asserts that it has been successful in saving lives.
Lynn recounts an example.
“I had just met this veteran a week before and I met all of his friends,” she said. “He turned out to be missing. He left a note and no one could find him but I remembered one person who knew who he was and what he does. So I called her and I said, ‘where would he be if he’s going to hide?’ and she told me exactly where he would be.
“I called the police and told them and they found him in time because he’d swallowed a whole bottle of Xanax and he was in the hills of Pennsylvania in the winter. So he would have frozen to death but he’s alive today still working on his stuff.”
Lynn said she believes her son would thank her for the foundation’s work.
She believes that, she said, because “he’s right by my side when I’m doing all this.”
The VA offers this advice:
To connect with a VA Veterans Crisis Line responder, anytime day or night:
Call 988 and select 1
Text 838255
Start a confidential chat: https://www.veteranscrisisline.net/get-help-now/chat/
If you have hearing loss, call TTY: 800-799-4889.
You can also take these actions:
Call 911.
Go to the nearest emergency room. Go directly to your nearest VA medical center. It doesn’t matter what your discharge status is or if you’re enrolled in VA health care.